Orthotics are
devices that are placed in the shoe to put the foot in a neutral
position, or provide cushioning depending on the type of orthotic.
Orthotics devices are used in foot conditions such as, flat foot, pes
cavus (high arched feet), equinus (muscular imbalance limiting upward
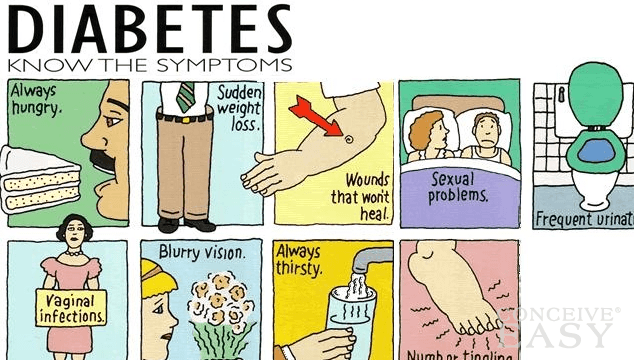
motion of foot), hammertoes, limb length difference, diabetes,
bunions and many other conditions. Orthotics can be custom made
or bought over the counter. A 3-dimensional scan of the foot is used
to send to a lab that makes custom made orthotics, and the orthotics
lab can add correction specific to the patients’ needs based on specific instructions in the form of a prescription from our offices.
Orthotics
fall into two different categories: functional and accommodative:
Functional orthotic devices are used to correct biomechanical
deformities in the frontal plane, and reduce impact while running or
walking. Functional correction is used to reduce
abnormal pronation by
providing support of the arch, while accommodative orthotics are a
soft supportive device used to provide cushioning, and distribute
weight bearing pressures evenly across the bottom of the foot.
When making orthotics it is important to compensate for limb length
differences because even a small difference can cause pathology, and
affect gait. Symptomatic differences in limb length usually
occur when there is a 4cm or greater difference. Functional
orthotics devices are made of semi-rigid material to provide
stability, such as graphite or plastic.
Accommodative orthotic devices are usually made of softer materials, such as leather or foam
to provide comfort. Accommodative orthotics devices are used in
conditions such as diabetes and rheumatoid arthritis to help relieve pressure and apply gentle offloading forces away from prominent structures of the foot.
This
is just a brief overview of the various uses and types of orthotics,
and is not complete by any means. For some people, orthotics
devices are a way to treat foot pain conservatively and avoid
surgery. Orthotics devices are sometimes recommended
post-operatively to prevent recurrence of various deformities.
However, some patients use orthotics devices to provide stability and
support to the foot, and prevent injuries.
Here, we have a 3-dimensional scanner which can allow us extremely accurate impressions of the feet in order to achieve both optimal comfort and control with our custom molded devices.

Orthotics,
also known as orthoses,
refers to any device inserted into a shoe, ranging from felt pads to
custom-made shoe inserts that correct an abnormal or irregular,
walking pattern. Sometimes called arch
supports,
orthotics allow people to stand, walk, and run more efficiently and
comfortably. While over-the-counter orthotic are available and may
help people with mild symptoms, they normally cannot correct the wide
range of symptoms that prescription foot orthoses can since they are
not custom made to fit an individual's unique foot
structure.
Orthotic devices come in many shapes, sizes,
and materials and fall into three main categories: those designed to
change foot function, those that are primarily protective in nature,
and those that combine functional control and protection.
Rigid
Orthotics
Rigid
orthotic devices are designed to control function and are used
primarily for walking or dress shoes. They are often composed of a
firm material, such as plastic or carbon fiber. Rigid orthotics are
made from a 3-dimensional scan of the foot or feet. Rigid orthotics control motion in the two
major foot joints that lie directly below the ankle joint and may
improve or eliminate strains, aches, and pains in the legs, thighs,
and lower back.
Soft
Orthotics
Soft
orthotics are generally used to absorb shock, increase balance, and
take pressure off uncomfortable or sore spots. They are usually
effective for diabetic, arthritic, and deformed feet. Soft orthotics
are typically made up of soft, cushioned materials so that they can
be worn against the sole of the foot, extending from the heel past
the ball of the foot, including the toes. Like rigid orthotics, soft
orthotics are also made from a 3-dimensional scan of the foot.
Semi-Rigid
Orthotics
Semi-rigid
orthotics provide foot balance for walking or participating in
sports. The typical semi-rigid orthotic is made up of layers of soft
material, reinforced with more rigid materials. Semi-rigid orthotics
are often prescribed for children to treat flatfoot
and in-toeing or out-toeing disorders.
These orthotics are also used to help athletes mitigate pain while
they train and compete.
If there is any question whether these sorts of devices may help you, most likely than can, because if you are questioning if you need them most likely your feet have some symptomatic concern which does require an evaluation.
Brian Timm, DPM, FACFAS
Board Certified by the American Board of Podiatric Surgery