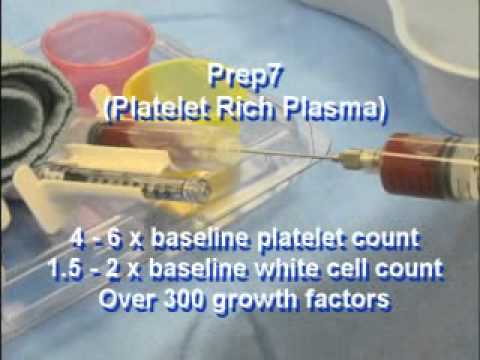
As the use of PRP increases, additional studies may establish PRP as an efficacious treatment modality and guide future treatment of chronic diabetic foot ulceration.
- Yale Journal of Biology and Medicine March 2010
We have been using PRP injections in this manner since 2010 as well, and this study was published promptly (and independently) from our center, but it shows the progressive mindset and improved outcomes from our center.
We are always striving to obtain the latest in technology to help treat our patients both effectively and not only by use of standard of care methods we will often go ABOVE the standard of care to ensure the most optimal in outcomes for our patients with diabetic wounds and neuropathic ulcerations.
McAleer et al. (2006) found that the use of autologous PRP was successful in healing a chronic lower extremity wound in a case study of a 57-year-old man with type 2 diabetes and a wound of six months duration.
Salemi et al. (2008) was a more recent case study evaluating the effectiveness of a combination of autologous adipose tissue and PRP in a lower extremity ulcer of three years duration in a non-diabetic 65-year-old male patient.
Margolis et al. (2001) was a retrospective cohort study devised to estimate the effectiveness of platelet releasate (PR) in the treatment of diabetic neuropathic foot ulcers. Of the 26,599 patients included in the study, 21 percent were treated with PR by the end of the 12-week run-in period before the 20-week study period began. The investigators concluded that PR was more likely to be used in more severe wounds and was also more effective in treating these wounds than the standard of care.
Driver et al. (2006) carried out the first reported prospective, randomized, controlled multicenter trial in the United States regarding the use of autologous PRP for the treatment of diabetic foot ulcers. Participants included 72 patients with type 1 and type 2 diabetes between the ages of 18 and 95 from 14 investigation sites suffering from an ulcer of at least four weeks duration. In this study, investigators compared the effectiveness of autologous PRP gel to that of normal saline gel for 12 weeks. The primary objective of this study was to evaluate the safety of PRP and the incidence of complete wound closure, defined as 100 percent re-epithelialization, when compared to the control treatment, and a secondary objective was rate of wound closure. Patients were randomized into two groups — standard of care with PRP gel or control (saline gel) — and were evaluated biweekly for 12 weeks. After excluding 32 patients from the final per-protocol analysis because of failure to complete treatment and protocol violations, the authors found that 68.4 percent (13/19) of patients in the PRP group and 42.9 percent (9/21) in the control group had wounds that healed. Wounds in the PRP group healed after a mean of 42.9 days (SD 18.3) vs. 47.4 days (SD 22.0) in the control group.
This is significant, because the longer the duration of time that there is an ulceration on the plantar skin the more directly proportional to likelihood of osteomyelitis formation occurs.
Metalink: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2844688/




No comments:
Post a Comment